Ovarian Cancer
Ovarian Cancer
Ovarian cancer (an insidious disease that is sometimes referred to as the “Whisper Killer”) is the fifth most common cancer among women.
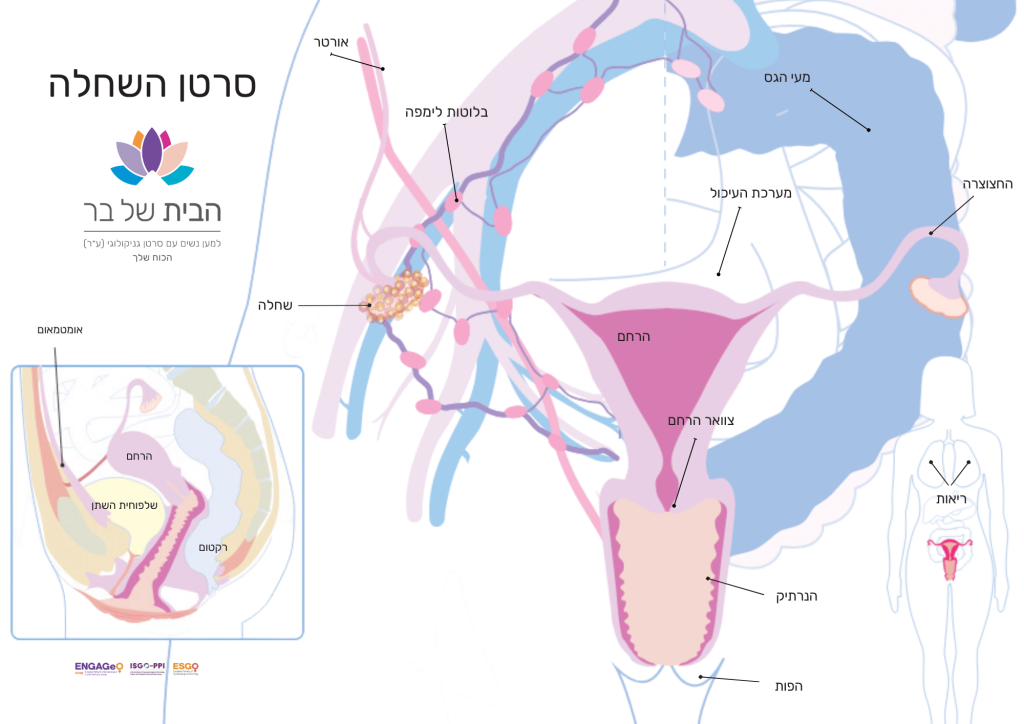
What Are the Ovaries?
The ovaries are two small, oval-shaped organs located in the pelvis (the area between the hips, at the lower part of the abdomen). They are part of the female reproductive system, which also includes the fallopian tubes, uterus, vagina, and vulva. During reproductive age, a mature egg is released from one of the ovaries each month and travels through a fallopian tube to the uterus. If the egg is not fertilized by sperm, it is expelled from the uterus, along with the uterine lining, as part of the monthly menstrual cycle. The ovaries also produce the female sex hormones estrogen and progesterone. As a woman approaches menopause, the ovaries produce fewer hormones, and menstruation gradually stops.
What Are the Symptoms of Ovarian Cancer?
- Nausea, gas, and digestive issues
- Persistent bloating
- Pelvic pain
- Frequent urination
- Loss of appetite or feeling full quickly
- Spotting or bleeding between periods
Diagnosis is typically initiated due to suspicious symptoms and includes:
- Physical and gynecological examination
- Imaging of the pelvis and abdomen (ultrasound, CT, PET-CT)
- Blood tests, including CA-125 protein levels
What is the Treatment for Ovarian Cancer?
Surgical Treatment
Treatment typically involves surgery to remove the tumor mass that has developed in the body, combined with chemotherapy to destroy cancer cells. Radiation therapy is less commonly used for this type of cancer.
Chemotherapy Treatment
Chemotherapy usually involves a combination of several drugs. Platinum salts and taxanes, known for decades to be effective against ovarian tumors, are the main components. The most common treatment for advanced ovarian cancer includes surgery followed by six cycles of a combination of carboplatin and paclitaxel.
What Happens After Treatment?
After chemotherapy, a clinical assessment of the disease is performed. If no evidence of disease is found, the patient will be monitored every three months for the first two years, with gradually increasing intervals thereafter. However, the disease may recur during or after chemotherapy. In such cases, a tailored treatment plan will be developed based on the patient’s condition.
What Happens After Treatment?
In recent decades, several chemotherapeutic drugs have been developed as additional lines of treatment. Ongoing clinical and preclinical trials are evaluating other drugs, including immunotherapies, genetic treatments, and more. In any case, a medication is discontinued if it does not prove effective.
Anthracycline Chemotherapy
The advantage of this drug lies in its relatively mild side effects. Unlike some other drugs, it does not cause hair loss, leads to less nausea and vomiting, causes less bone marrow suppression, and has a lower risk of cardiac toxicity. However, it can cause more skin and mucous membrane side effects, which can be reduced with appropriate measures.
This drug is also used in breast cancer treatment, and due to its lower cardiac toxicity it is particularly recommended for women at high risk of developing heart disease. They include women with existing heart conditions, high blood pressure, a history of chest radiation or similar treatments, and older women.
Angiogenesis Inhibitors (ANTI-VEGF)
Another drug in use is an antibody that blocks the formation of new blood vessels around the tumor. Cancerous tumors rely on recruiting new blood vessels to ensure a continued supply of oxygen and nutrients for their growth.
New Generation of Drugs – PARP Inhibitors
A new generation of drugs includes PARP inhibitors. Women with a BRCA1/2 gene mutation lack a functional BRCA gene, which is crucial for DNA repair and cell survival. PARP is a protein that helps repair DNA damage in cells. Since cancer cells have DNA defects, they rely on PARP for repair. The drug blocks PARP, preventing the repair of cancer cells’ DNA damage, leading to cell death, thereby halting or shrinking the tumor.
Not Just for BRCA Mutation Carriers – Ask Your Doctor About the HRD Test
The HRD (Homologous Recombination Deficiency) test is a pathological examination of the tumor tissue. HRD is defined by the tumor’s inability to accurately repair double-strand DNA breaks through homologous recombination.
HRD can be assessed using two different types of biomarkers. In ovarian cancer, these include individual mutations in BRCA-related genes and an assessment of genomic instability. Genomic instability, or large-scale structural rearrangements of chromosomes, leads to specific measurable genomic deviations. Tumor samples with either BRCA1/2 mutations or genomic instability markers are characterized as HRD positive. Patients who are HRD positive are eligible for treatment with PARP inhibitors.
Hope is Here
Although ovarian cancer is often detected at a late stage, it is important to remember that recent years have seen significant advancements in available treatment methods, along with increased cure rates and average life expectancy for patients. Awareness and adherence to regular gynecological check-ups are key to early diagnosis and improved chances of recovery. New medications introduced in the past two decades, such as Avastin (an anti-VEGF) and PARP inhibitors, bring renewed hope, with the latter even altering the course of the disease.
We make every effort to provide evidence-based and reliable health information. We invest significant time and resources to ensure the information on our website is as accurate and up-to-date as possible, supported by scientific sources and aligned with current professional knowledge in relevant fields. However, the information in this website does not constitute medical advice or recommendations. We encourage anyone seeking personalized advice or recommendations on medical matters to consult directly with a licensed physician or a certified healthcare professional in the relevant field.