Vulvar Cancer
Vulvar Cancer
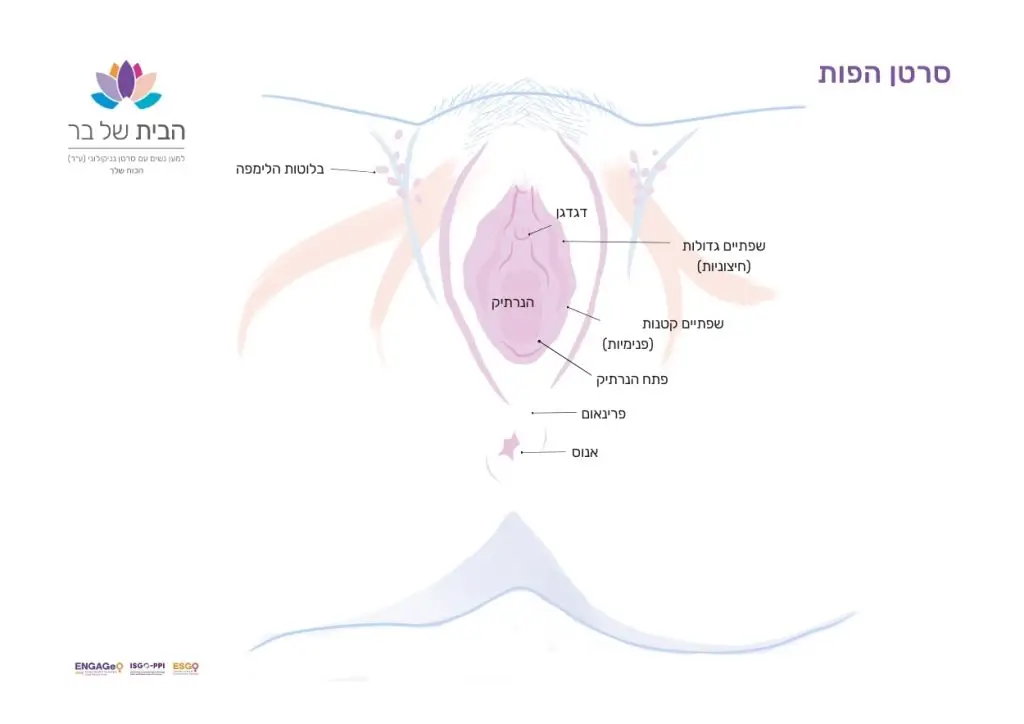
Vulvar cancer is a type of cancer that develops on the skin surrounding the urethra and vagina, including the clitoris and labia. It appears as a lump or sore on the vulva that does not heal and often causes itching. While it can occur at any age, it is usually diagnosed in older women.
Vulvar cancer typically develops slowly over time. Before malignancy appears, early changes occur in the cells, often referred to as “precancerous changes,” which may develop into cancer if not properly treated.
Risk Factors:
Vulvar cancer is a type of cancer that develops on the skin surrounding the urethra and vagina, including the clitoris and labia. It appears as a lump or sore on the vulva that does not heal and often causes itching. While it can occur at any age, it is usually diagnosed in older women.
Vulvar cancer typically develops slowly over time. Before malignancy appears, early changes occur in the cells, often referred to as “precancerous changes,” which may develop into cancer if not properly treated.
Warning Signs:
- Itching
- Burning sensation and pain in the vulva
- Lump, swelling, or wart appearance
- Thickened, raised, red, white, or dark areas on the vulvar skin
- Bleeding or bloody discharge
- Burning pain during urination
- Increased sensitivity and pain in the vulva
- Sore or ulcer on the vulva
- Mole on the vulva that changes shape or color
How Is Vulvar Cancer Diagnosed?
Diagnosis involves a physical and gynecological exam, colposcopy, and biopsy. Imaging of the pelvis and abdomen (ultrasound, CT, or PET-CT) is also performed, along with blood tests, including liver and kidney function tests.
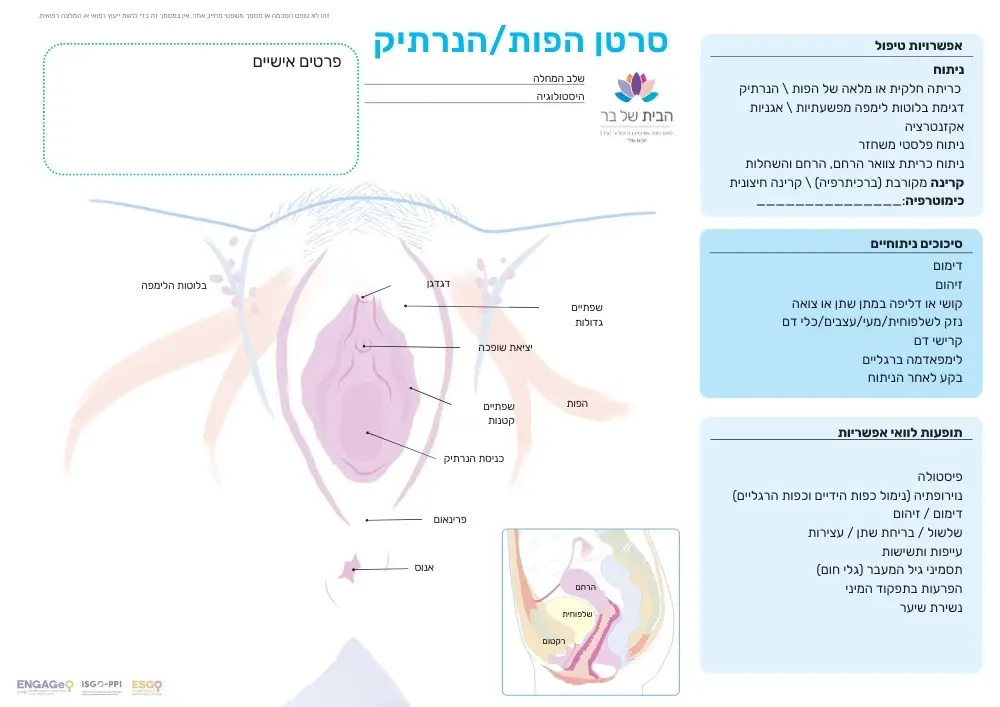
Treatment for Vulvar Cancer
Treatment typically involves surgery to remove the tumor and assess microscopic spread that is not visible, such as involvement of the lymph nodes. Additional surgeries may include complete removal of the vulva and inguinal lymph nodes. In cases of advanced vulvar cancer, pelvic exenteration may be performed to remove all affected organs (such as the cervix, uterus, and ovaries).
In appropriate cases, additional treatment after surgery may include external radiation, internal radiation (brachytherapy), and chemotherapy (such as cisplatin or fluorouracil). Sometimes, chemotherapy is given alongside radiation therapy, as certain types of chemotherapy enhance the effects of radiation. A combination of low-dose chemotherapy and radiation can be used to improve the tumor’s response to radiotherapy. Read more about radiation therapy here.
We make every effort to provide evidence-based and reliable health information. We invest significant time and resources to ensure the information on our website is as accurate and up-to-date as possible, supported by scientific sources and aligned with current professional knowledge in relevant fields. However, the information in this website does not constitute medical advice or recommendations. We encourage anyone seeking personalized advice or recommendations on medical matters to consult directly with a licensed physician or a certified healthcare professional in the relevant field.
Navigation
Postal address:
Shmu’el Shnitser St 3, Tel Aviv 6958312