Cervical Cancer

Have you been diagnosed with cervical cancer?
Help us fight for your rights! We advocate for the rights of anyone diagnosed with cervical cancer or precancer. We've created a survey to highlight the challenges faced after treatment. It only takes a few minutes to complete, but it’s crucial! This is how we can make a change. Please take a moment to help us ensure a better future for all patients.
Cervical Cancer
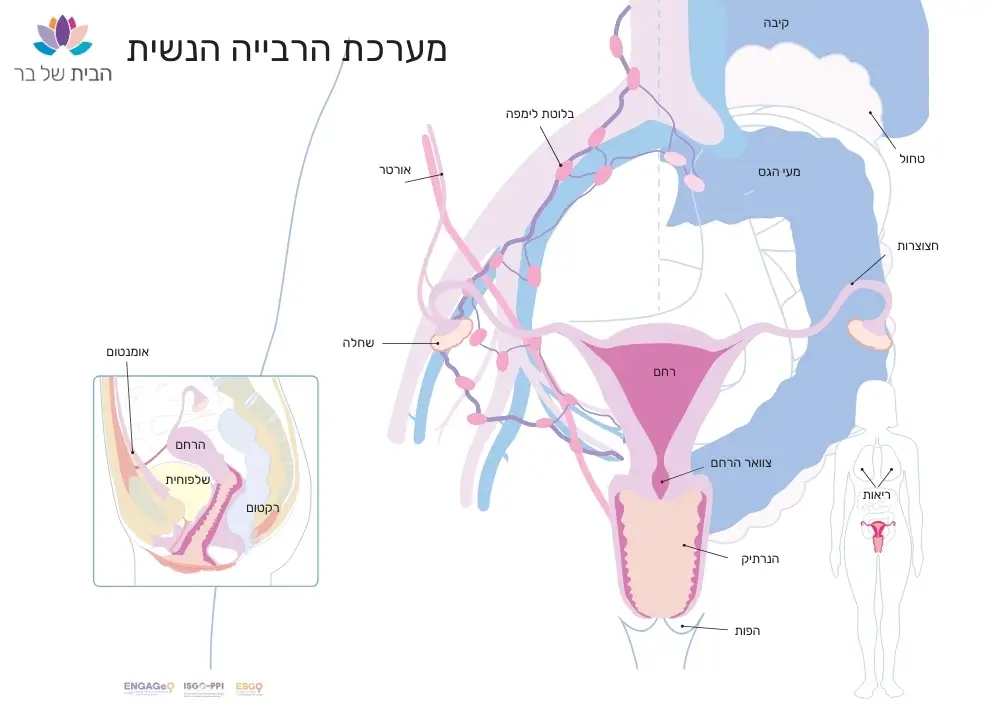
The cervix is part of the female reproductive system, which includes the ovaries, fallopian tubes, uterus, vagina, and vulva. The cervix connects the uterus to the vagina.
Roles of the Cervix:
- Produces moisture to lubricate and maintain vaginal health.
- Opens to allow menstrual blood to flow from the uterus to the vagina.
- Produces mucus that helps sperm travel up the uterus and fallopian tubes, on its way to fertilize an egg released from the ovary.
- Holds a developing baby in the uterus during pregnancy by remaining closed, then dilates to allow the baby to be born through the vagina.
Routine Screening Tests for Cervical Cancer:
- Pap Test – A Pap smear is a screening test to detect early precancerous changes in the cervix. It is performed during routine gynecological exams for all women. Professional guidelines recommend a Pap test every three years for women aged 30-65.
- HPV Typing Test – This PCR test detects the human papillomavirus (HPV) in the cervical area and identifies high-risk HPV strains that could cause precancerous changes. It is taken along with the Pap test as part of routine screening for women aged 25 and older. Adding HPV testing increases the sensitivity of cervical cancer screening.
What is Cervical Cancer?
Cervical cancer typically develops slowly over time. Before malignancy appears in the cervix, early changes occur in the cells, known as “precancerous changes.” These are cells that may develop into cancer if not properly treated.
Cervical cancer is almost entirely preventable by reducing risk factors
Risk Factors for Cervical Cancer:
- HPV – In Israel, around 280 new cases of cervical cancer are diagnosed each year, with 95% of them caused by HPV. Read more about HPV here.
- Age
- Smoking
- Immunodeficiencies
Cervical cancer is the fourth most common cancer among women in Israel and worldwide. In Israel, its prevalence is lower than in many other countries, with 5 cases per 100,000 women. It typically appears in two main age groups: 35-39 and 60-64. However, the risk exists at any age, so regular gynecological check-ups are important.
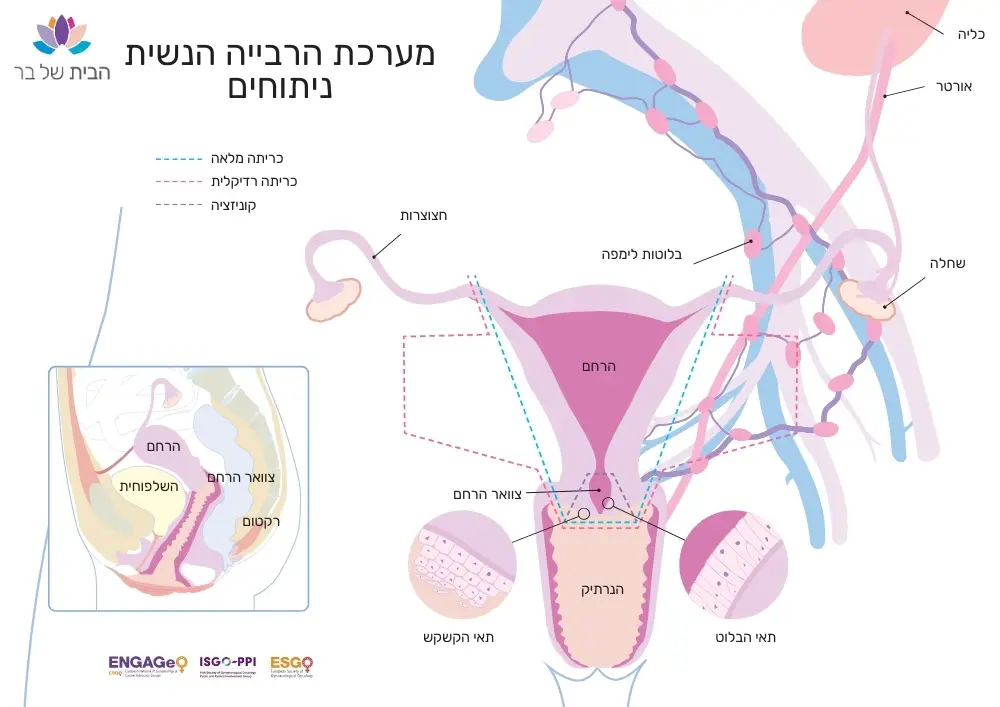
Types of cervical cancers are named after their cells of origin:
Squamous Cell Carcinoma – Arises from flat, thin cells covering the outer surface of the cervix (ectocervix). It accounts for about 70-80% of all cervical cancer cases.
Adenocarcinoma – Develops from column-shaped cells lining the inner surface of the cervix (cervical canal or endocervix). Adenocarcinoma, which makes up about 25% of cases, begins in the glandular cells of the cervix. It is more challenging to diagnose because it occurs higher up in the cervix, making abnormal glandular cells harder to detect.
Adenosquamous Carcinomas – A small number of cervical cancers involve both squamous and glandular cells. These are known as adenosquamous or mixed carcinomas. Other rare types of cancer that can start in the cervix include small cell carcinoma and cervical sarcoma.
Diagnosis of Cervical Cancer
Diagnosis of cervical cancer is typically made following suspicious symptoms, and is based on physical and gynecological exams, colposcopy, biopsies obtained through curettage or conization, imaging of the pelvis and abdomen (ultrasound, CT, or PET-CT), and blood tests including liver and kidney function tests.
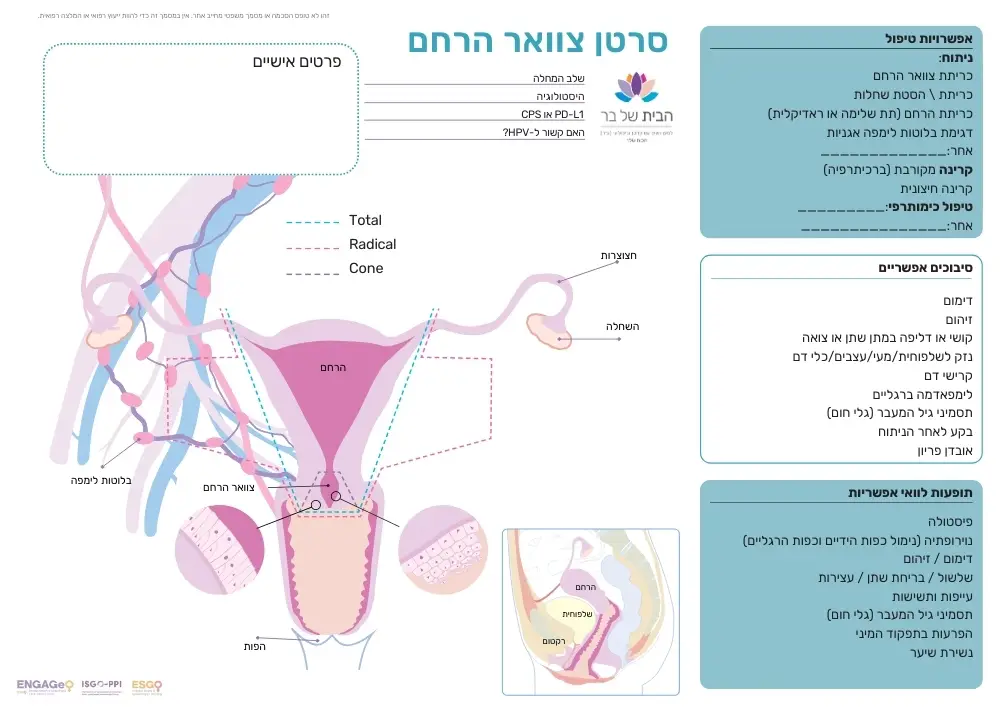
Treatment for Cervical Cancer
The decision on the treatment approach for cervical cancer is made after a comprehensive evaluation by the medical team.
Surgical Treatment
Treatment for cervical cancer often involves surgery to remove the tumor and gather information about any microscopic spread of the disease, such as undetectable cancer in the lymph nodes. Read more.
Radiation Therapy
External Radiation (Radiotherapy): Uses powerful X-rays to target the tumor, damaging cancer cells during division, which can shrink or even destroy the tumor. Radiation planning with a simulation (cross-sectional imaging of the treated area) is done to ensure precision. The treatment is typically given five days a week for four to six weeks.
Internal Radiation (Brachytherapy): Delivers radiation directly into the tumor through the vagina using carriers, usually under epidural anesthesia.
Side effects may include mild vaginal bleeding, abdominal pain (manageable with painkillers like Tylenol or Advil), a burning sensation during urination (proper hydration and painkillers are recommended for relief), and skin discoloration around the vulva, abdomen, and thighs. Seek emergency care for heavy bleeding (a full night pad every two hours), fever above 37.8°C (100°F), or severe abdominal pain.
Systemic Therapy
Chemotherapy is sometimes administered alongside radiation, as certain chemotherapy drugs enhance the effect of radiation. In cervical cancer, a combination of low-dose chemotherapy and radiation can be used to improve tumor response to treatment.
Treatment for Metastatic Cervical Cancer
Patients with metastatic cervical cancer may be eligible for immunotherapy or biological therapy. Read more here….
We make every effort to provide evidence-based and reliable health information. We invest significant time and resources to ensure the information on our website is as accurate and up-to-date as possible, supported by scientific sources and aligned with current professional knowledge in relevant fields. However, the information in this website does not constitute medical advice or recommendations. We encourage anyone seeking personalized advice or recommendations on medical matters to consult directly with a licensed physician or a certified healthcare professional in the relevant field.
Navigation
Postal address:
Shmu’el Shnitser St 3, Tel Aviv 6958312