Surgery
A hysterectomy is a surgical procedure to remove the uterus and may be recommended for women diagnosed with cervical cancer, ovarian cancer, fallopian tube cancer, or endometrial cancer. If the cancer has spread to an advanced stage, chemotherapy may be suggested before surgery.
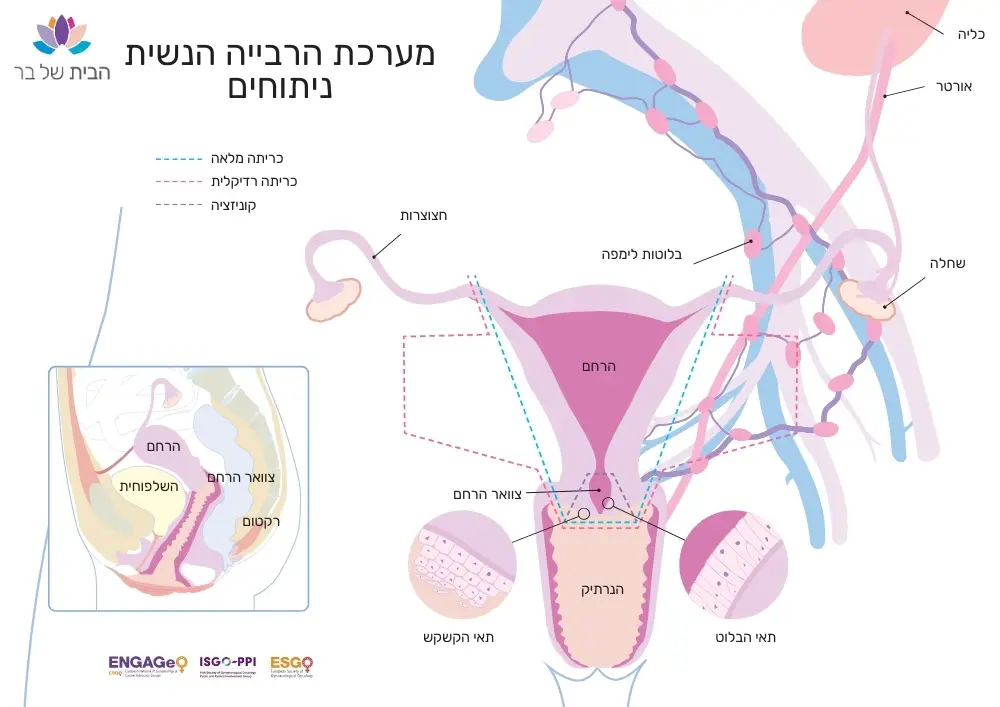
There are several techniques for performing a hysterectomy. The choice of procedure depends on the tumor size, your age, medical condition, and family planning considerations:
Subtotal Hysterectomy
Involves removing the main body of the uterus while leaving the cervix intact. This procedure is less common. If the cervix remains, there is still a risk of cervical cancer, requiring regular cervical screening.
Total Hysterectomy
Usually recommended for patients with endometrial cancer, ovarian cancer, or those with cervical pre-cancer or cancer who have completed childbearing. This procedure involves removing both the uterus and cervix. It is generally preferred over a subtotal hysterectomy due to a lower risk of residual disease when the cervix is removed.
Cervical Removal (Trachelectomy)
If you have pre-cancerous lesions or cervical cancer, removing the cervix may be recommended to prevent the spread of cancer. After removal, samples for Pap smears will be taken from the vagina or vulva.
(BSO: Bilateral Salpingo-Oophorectomy)
Oophorectomy
The ovaries produce eggs that travel to the fallopian tube, are fertilized, and continue to develop in the uterus. At menopause, the maturation of eggs ceases, and menstruation stops. Ovaries may develop conditions requiring treatment, such as ovarian cancer, which is treated through oophorectomy and systemic treatments like chemotherapy.
In cases where ovarian cancer is detected at a young age, preserving a healthy ovary may be considered. However, in most cases, both ovaries and fallopian tubes are removed to prevent any remaining tissue from developing cancer. If you have not completed your family planning and are diagnosed with ovarian cancer, consulting a fertility specialist is advised.
Preventive Oophorectomy
The National Institute for Health and Care Excellence (NICE) recommends removing a woman’s ovaries and fallopian tubes (adnexa) only if there is a significant risk factor, such as carrying the BRCA gene mutation. If you have a family history of ovarian or breast cancer or carry the BRCA gene mutation, preventive removal of the ovaries and fallopian tubes may be recommended. It is important to discuss the benefits and risks with your gynecologic oncologist. Some surgeons suggest removing only the fallopian tubes since the ovaries produce hormones that can protect against health issues like osteoporosis and play a role in sexual desire and pleasure.
Laparoscopic Surgery
Also known as keyhole surgery, this is the preferred method for removing organs and surrounding tissues of the reproductive system. During the procedure, a small tube containing a telescope (laparoscope) and a tiny video camera is inserted through a small incision in your abdomen, allowing the surgeon to view your internal organs. Other instruments are inserted through small incisions in the abdomen or vagina to remove the uterus, cervix, or any other part of the reproductive system.
Vaginal Surgery (VNOTE)
In a vaginal hysterectomy, the uterus and cervix are removed through an incision made at the top of the vagina. Special surgical instruments are inserted into the vagina to detach the uterus from the ligaments holding it in place. After removing the uterus and cervix, the incision is stitched. This procedure typically takes about an hour and is less invasive, involving a shorter hospital stay and faster recovery time.
Abdominal Surgery (Open Surgery Approach)
During this surgery, an incision is made in the abdomen, either horizontally along the bikini line or vertically from the navel to the bikini line. An open surgery approach may be recommended if the pelvic tumor cannot be removed through the vagina.
Meet with the anesthesiologist – Schedule a pre-surgery consultation with the anesthesiologist, where you can discuss recovery from general anesthesia and clarify fasting instructions.
Ask your surgeon about recovery time – Recovery from a vaginal surgery differs from that of open abdominal surgery. It is essential to get complete information from your surgeon to prepare for the expected recovery period.
Check if you need to remove gel nail polish or jewelry – Confirm whether these should be removed before surgery.
Ask if you need to bring your regular medications to the hospital – It’s usually recommended to bring any medications you take regularly at home.
Inquire about any special bathing instructions – Check if there are specific guidelines for bathing before surgery.
The medical staff will have inserted a urinary catheter – a small tube that drains urine from your bladder into a collection bag.
You may have a drainage tube in your abdomen, which typically remains in place for a few days until removed.
If you had a vaginal hysterectomy, a gauze strip may have been inserted into your vagina, which will be removed about 24 hours after surgery.
Constipation is a very common side effect after surgery. Although it doesn’t always occur, it’s essential to be aware that surgery can lead to constipation, characterized by difficulty and pain during bowel movements, fewer than three bowel movements per week, and dry, lumpy stool. If you experience constipation, it is crucial to inform the nursing staff and your doctors, as you need to pass stool before being discharged from the hospital.
The day after surgery, you will be encouraged to take a short walk to promote blood circulation and reduce the risk of complications like blood clots in the legs (deep vein thrombosis). A physiotherapist may show you some exercises to help with mobility.
It’s advisable to request a referral for pelvic floor physiotherapy to help strengthen your pelvic muscles during recovery.
Stitches are usually removed 5 to 7 days after surgery. You may be asked to return for a follow-up appointment with your surgeon 4 to 6 weeks after surgery.
Full recovery after an open abdominal surgery typically takes about 6 to 8 weeks, and recovery times are usually shorter after a vaginal or laparoscopic hysterectomy. During this time, rest as much as possible and avoid lifting heavy objects, as your abdominal muscles and surrounding tissues need time to heal.
Ask your doctors for precise guidelines!
If you live alone, it is essential to inform the hospital, request to speak with the department’s social worker, and apply for special services with social welfare.
This list was compiled from recommendations by women in our community:
Every day gets better, and each day of recovery is different…
- Check with your surgeon how long your hospitalization might be, so you can prepare your household accordingly.
- I stayed in the hospital for 6 days; I could only eat a little starting from the third day, and barely ate anything the first two days.
- Dates and prunes (you’ll thank me later)!
- Comfortable and warm clothing, it’s cold in the hospital.
- Loose and airy dress or tunic for discharge.
- A robe, though the hospital gown was the most comfortable for me.
- Cozy slippers that are easy to slip on without help.
- Body and face towels.
- Eye mask (helped me a lot).
- Earplugs (the woman next to me snored at night).
- Warm socks.
- Comfortable sandals for walking, flip-flops are less recommended.
- Favorite blanket or pillow, a cozy throw from home.
- Abdominal belt (recommended, but not for the first day or two), you can consult with your doctor on this recommendation.
- Books, magazines, a coloring book, and markers.
- Charger (I forgot mine, not a good idea).
- Headphones that connect to the hospital TV.
- Lip balm.
- Water bottle with a straw.
- Toiletries.
- Personal care items – sometimes, after the initial shock of surgery, you want to feel human and feminine again. A bit of perfume, face cream, or a little lipstick can do the trick.
- Soap and shampoo from home.
- Anything that lifts your spirits, like a nice-smelling soap, lotions, chocolates, music…
- Patience and a willingness to accept help. Basically, anything that brings a bit of joy
We make every effort to provide evidence-based and reliable health information. We invest significant time and resources to ensure the information on our website is as accurate and up-to-date as possible, supported by scientific sources and aligned with current professional knowledge in relevant fields. However, the information in this website does not constitute medical advice or recommendations. We encourage anyone seeking personalized advice or recommendations on medical matters to consult directly with a licensed physician or a certified healthcare professional in the relevant field.
Navigation
Postal address:
Shmu’el Shnitser St 3, Tel Aviv 6958312