Cancer Treatment
Radiotherapy
External Radiation (Radiotherapy):
This treatment uses powerful X-rays to penetrate the tumor area, damaging cancer cells during their division, which can shrink or destroy the tumor. To maximize effectiveness, radiation planning is done using a simulation—a cross-sectional scan of the treated area to precisely mark the radiation target. Typically, external radiation therapy is given five days a week for four to six weeks, with each treatment session lasting about 10 minutes.
Internal Radiation (Brachytherapy):
Brachytherapy delivers a higher dose of radiation directly to the tumor, reducing radiation exposure to surrounding healthy tissues such as the intestines and bladder. This treatment complements external radiation and is crucial for achieving a cure.
While the external radiation plan is consistent throughout the treatment days, brachytherapy is planned on the same day of treatment based on a simulation performed at the time, allowing for much greater precision and significantly increased treatment effectiveness.
Brachytherapy typically begins two to three weeks after starting external radiation. The number of treatments ranges from four to five, given once or twice a week. It is essential to maintain this schedule without delays to achieve the most effective results.
In most cases of cervical cancer, brachytherapy is therapeutic.
In most cases of endometrial cancer, brachytherapy serves as preventive radiation, providing a boost to prevent cancer recurrence.
General Anesthesia During Applicator Placement:
General anesthesia is administered only during the placement of the applicator. Once the applicator is in place, you are moved to the recovery room and awakened from anesthesia (general anesthesia requires the presence of an anesthesiologist in an operating room). Upon waking you may begin to feel discomfort, and the medical team typically provides pain relief to help manage this sensation.
Spinal Anesthesia:
The main difference between the two types of anesthesia is that spinal anesthesia lasts about 3 hours (covering the entire treatment), while general anesthesia lasts only 20 minutes (during applicator placement). After 20 minutes, pain medications are provided as needed based on your pain level.
Although spinal anesthesia might seem intimidating, the injection takes only about 10 seconds, after which you typically feel very little for an extended period.
LDR (Low-Dose Rate) – Radiation is delivered at a low dose over several days.
HDR (High-Dose Rate) – Radiation is stronger, with each treatment lasting a very short time, typically only 5 to 20 minutes.
In Israel, HDR is commonly used.
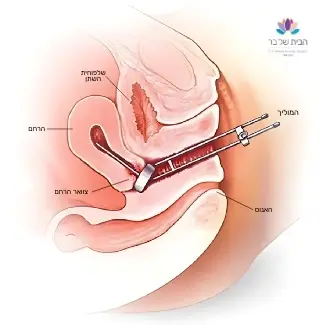
In brachytherapy, radiation applicators are used to deliver radiation precisely to the tumor area. There are several types of applicators, and the physician selects the most appropriate one based on the treatment goal, tumor location, and medical condition.
Types of Applicators:
PLV (Partial-Length Vaginal) Brachytherapy
FLV (Full-Length Vaginal) Brachytherapy
Depending on the applicator type, the procedure may be performed with or without local or general anesthesia to prevent pain.
Before Your First Brachytherapy Session Before your first brachytherapy treatment, you will need to meet with an anesthesiologist. This appointment should be scheduled after you have completed a urine test, blood tests, and an ECG. Following your meeting with the anesthesiologist, you will undergo the remaining necessary tests with the guidance and support of the medical team at your treatment center. Each time before a brachytherapy session, 1-2 days in advance, you will need to have blood tests (similar to those required before chemotherapy). It is recommended to send the test results to the secretary or nurse at the clinic where you are being treated and confirm that the results allow you to proceed with the brachytherapy on the scheduled date. |
On Treatment Day Though the procedure may vary slightly between clinics, we will be discussing international guidelines here. In most clinics, brachytherapy is performed in the afternoon, which helps facilitate a smooth treatment process since most external radiation treatments are given in the morning. You will receive specific instructions from your clinic about fasting times for food and drink. Preparation at Home: Fasting:
Bowel Preparation: |
Treatment Process The entire treatment, from admission to discharge, usually takes about 3-4 hours. It is important to arrive at the clinic on time to help reduce the duration of the session and wait times for yourself and for other patients receiving brachytherapy that day.
On treatment day you will:
|
After the treatment:
You may experience spotting, bleeding, or vaginal discharge after the applicator is removed. It is recommended to bring an absorbent pad.
You might have cramps similar to menstrual pain for up to 24 hours after the procedure. You can use pain relievers to alleviate the cramps.
You may feel a burning sensation when urinating for up to 24 hours. It is advisable to drink 8-10 glasses of water a day.
Some may experience diarrhea.
It is recommended to avoid sexual intercourse during treatment due to possible vaginal sensitivity and irritation.
You are not radioactive in any way after the procedure, and can safely be around family and friends.
You can eat normally and continue your regular activities throughout the treatment.
When to Seek Emergency Care
You should go to the emergency room if:
You develop a fever above 37.8°C (100°F) within 48 hours after the treatment.
You experience pain that does not subside with pain relievers.
You have heavy bleeding, such as filling a night pad within two hours.
You notice a burning sensation or blood in your urine lasting more than 24 hours after the procedure.
You have not had a bowel movement for 3-4 days after the procedure.
When to Seek Emergency Care
You should go to the emergency room if:
- You develop a fever above 37.8°C (100°F) within 48 hours after the treatment.
- You experience pain that does not subside with pain relievers.
- You have heavy bleeding, such as filling a night pad within two hours.
- You notice a burning sensation or blood in your urine lasting more than 24 hours after the procedure.
- You have not had a bowel movement for 3-4 days after the procedure.
We make every effort to provide evidence-based and reliable health information. We invest significant time and resources to ensure the information on our website is as accurate and up-to-date as possible, supported by scientific sources and aligned with current professional knowledge in relevant fields. However, the information in this website does not constitute medical advice or recommendations. We encourage anyone seeking personalized advice or recommendations on medical matters to consult directly with a licensed physician or a certified healthcare professional in the relevant field.
Navigation
Postal address:
Shmu’el Shnitser St 3, Tel Aviv 6958312