Endometrial Cancer
Endometrial Cancer
The cancer that can be detected early.
Uterine cancer is the most common gynecological cancer. It is usually diagnosed early and successfully treated. 95% of endometrial cancers develop from the uterine wall, and include uterine carcinomas and adenocarcinomas.
Factors that might increase the risk of endometrial cancer include:
- Age – As with most cancers, the risk of developing endometrial cancer increases with age.
- Obesity and Lack of Physical Activity – Obesity is a significant risk factor, as fat tissue produces estrogen, a hormone that can increase the risk of endometrial cancer. About 70% of endometrial cancer cases are linked to obesity, and this type of cancer is twice as common among overweight women.
- Hormonal Factors – A hormone imbalance where estrogen levels exceed progesterone levels can raise the risk of endometrial cancer.
Warning Signs?
If you experience one of the following symptoms of endometrial cancer, consult a healthcare provider.
- Abnormal vaginal bleeding
- Excessive menstrual bleeding
- Postmenopausal vaginal bleeding
- Pelvic pain
- Abnormal vaginal discharge
- Unintentional weight loss
- Palpable pelvic mass
- Disruption of bladder function (urinary retention or incontinence)
Diagnosis
The diagnosis is typically made following suspicious symptoms and is based on physical and gynecological exams, biopsies performed via pipelle or hysteroscopy, imaging of the pelvis and abdomen (ultrasound, CT, or PET-CT), and blood tests including liver and kidney function and CA-125 protein levels.
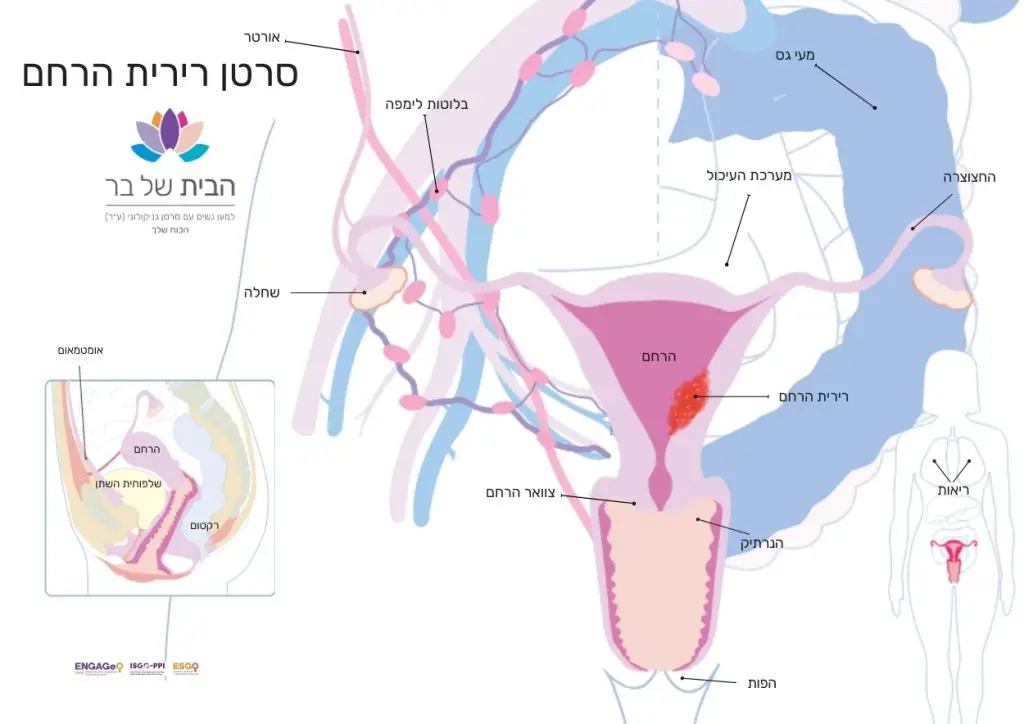
What is the Uterus?
The uterus is a muscular organ located at the top of the cervix, where the fetus develops during pregnancy.
The uterus is composed of three layers:
- Endometrium – The inner lining
- Myometrium – The thickest layer, comprising mostly muscle
- Serosa – The thin outer layer
During a woman’s reproductive years, if pregnancy does not occur, the endometrial lining is shed through the vagina (menstruation). This process continues until menopause, when the ovaries stop releasing eggs, and the endometrium becomes thin and inactive.
The uterus is supported by the pelvic floor muscles.
Uterine Cancer
Endometrial cancer is often detected early and is usually fully curable. Early detection, along with significant advances in available treatment options, offers real hope to patients. Awareness and consistent and regular gynecological check-ups are key to early diagnosis, improving the chances of recovery and successful treatment.
Types of Uterine Tumors:
Adenocarcinoma: This tumor originates in the inner lining of the uterus (endometrium) and is known as endometrial adenocarcinoma. It is usually diagnosed at an early stage and has high cure rates. The most common subtype is endometrioid carcinoma. Less common subtypes include serous carcinoma, the rare clear cell adenocarcinoma, and carcinosarcoma, which is a mix of adenocarcinoma and sarcoma.
Uterine Sarcoma: This type of cancer develops in the supporting tissues of the uterine glands or in the myometrium, the muscular layer of the uterus, rather than in the endometrium. Uterine sarcomas account for about 2% to 4% of uterine cancer cases. Subtypes include leiomyosarcoma (the most common subtype), endometrial stromal sarcoma, and undifferentiated sarcoma.
Staging of Endometrial Cancer
Treatment for endometrial cancer is determined based on the stage of the disease. In 2022, the International Federation of Gynecology and Obstetrics (FIGO) updated the staging system for endometrial cancer. The staging system classifies the size and spread of the cancer, helping doctors decide on the appropriate treatment and its duration. The major updates include incorporating risk stratification, histological features, growth patterns, and even molecular classifications. Below is the updated staging system for endometrial cancer:
Stage I - Confined to the uterine corpus and ovary
|
|
|
Stage II - Invasion of cervical stroma without extrauterine extension OR with substantial LVSI OR aggressive histological types with myometrial invasion
|
|
|
Stage III - Local and/or regional spread of the tumor of any histological subtype
|
|
|
Stage IV - Spread to the bladder mucosa and/or intestinal mucosa and/or distance metastasis
|
|
|
* Histology is the scientific field that studies the structure of living tissues. It involves identifying, examining under a microscope, and analyzing these tissues. Histology is essential in medicine as it allows doctors to diagnose diseases and monitor treatments. Additionally, histology plays a crucial role in scientific research, helping to understand the structure and function of tissues.
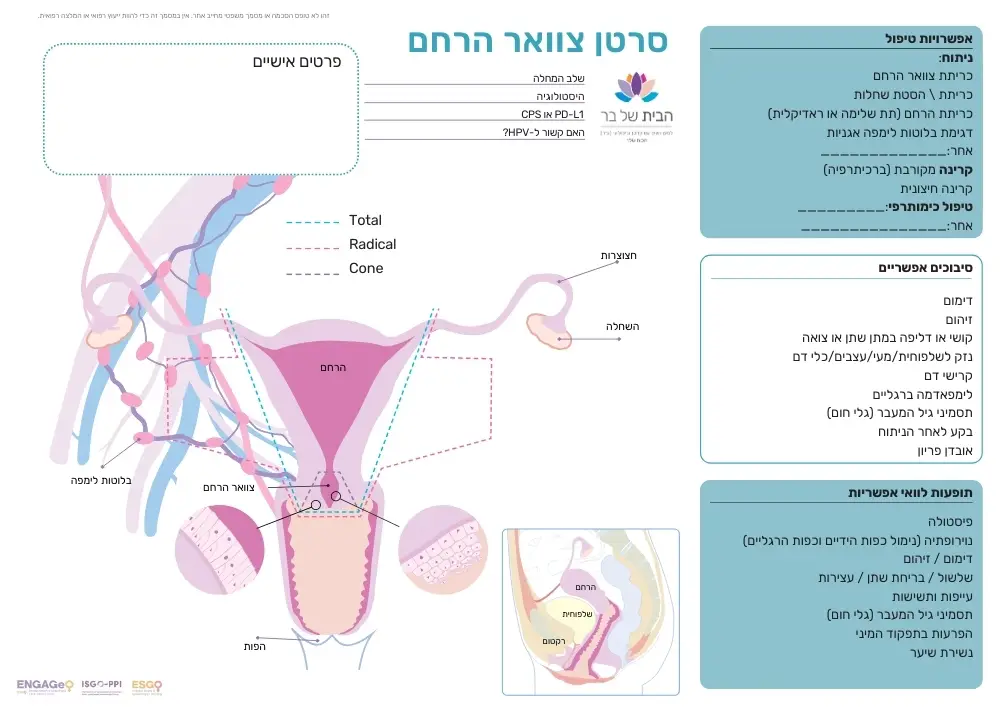
Treatment for Endometrial Cancer
Surgery – In most cases, the disease can be cured with surgery aimed at removing the tumor. Typically, this involves a hysterectomy (removal of the uterus), and sometimes also the removal of the fallopian tubes and ovaries. Read more about surgeries here.
Radiation Therapy – Sometimes radiation is necessary, either as external radiation or vaginal brachytherapy. Read more about radiation therapy here.
Chemotherapy – During surgery, biopsy samples are taken from lymph nodes to determine the stage of the disease. If the tumor has spread to the lymph nodes or if the tumor’s histology is unique, chemotherapy may be included in the treatment plan to destroy cancer cells. Chemotherapy typically involves a combination of drugs. Platinum salts and taxanes, long proven to be effective in treating uterine tumors, are the primary components. Read more about chemotherapy here.
For advanced uterine cancer, the standard treatment includes surgery followed by a combination of two chemotherapy drugs (Carboplatin and Taxol) administered in six cycles.
After chemotherapy, a clinical evaluation of the disease is performed. If no signs of the disease are present, the patient is monitored every three months for the first two years and then at increasing intervals.
However, recurrence can happen during or after chemotherapy. In such cases, additional chemotherapy or immunotherapy might be necessary. Over the past few decades, several drugs have been developed for subsequent lines of treatment.
Innovation in Endometrial Cancer
Immunotherapy
Patients with metastatic or recurrent endometrial cancer whose tumors are MSI-H (microsatellite instability-high) or dMMR (deficient mismatch repair) are eligible for immunotherapy. This treatment is available through the “healthcare basket” as a second-line option, meaning it is offered after chemotherapy for those needing continued treatment.
Patients whose tumors are pMMR (proficient mismatch repair) may receive immunotherapy in combination with targeted therapy, specifically with tyrosine kinase inhibitors (TKIs).
Targeted Therapy
Tyrosine kinase inhibitors (TKIs) work through two main mechanisms to block cancer cell growth while minimizing damage to healthy cells. These include disrupting a protein that promotes cancer cell division, thereby slowing tumor growth, and blocking the VEGF receptor, which is responsible for supplying blood to the cancer cells, cutting off the tumor’s nutrient source.
Biological Therapy
Another commonly used drug is Avastin, an anti-angiogenesis medication. It is an antibody that blocks the formation of new blood vessels around the tumor. Cancerous tumors rely on recruiting new blood vessels to ensure a continued supply of oxygen and nutrients for their growth.
We make every effort to provide evidence-based and reliable health information. We invest significant time and resources to ensure the information on our website is as accurate and up-to-date as possible, supported by scientific sources and aligned with current professional knowledge in relevant fields. However, the information in this website does not constitute medical advice or recommendations. We encourage anyone seeking personalized advice or recommendations on medical matters to consult directly with a licensed physician or a certified healthcare professional in the relevant field.
Navigation
Postal address:
Shmu’el Shnitser St 3, Tel Aviv 6958312